Lydia Nunez Landry,
Certified Long-Term Care Ombudsman
disabled disability advocate
Submitted for the United States Committee on Finance record at a hearing on:
A National Tragedy: COVID-19 in the Nation’s Nursing Homes
Wednesday, March 17, 2021
Chairman Wyden, Ranking Member Crapo, and distinguished Members of the Committee,
My name is Lydia Nunez Landry and I am writing to you today not as someone the American Health Care Association and LeadingAge would reduce to the characterization (in their ‘Care for Our Senior’s Act’) of a “frail [or] elderly adult with underlying health conditions” at risk of dying from COVID “630 times higher than an 18 to 29” year old, that is, someone these lobbyists designate as prone to death. Rather, despite reductions of people like me—or any other marginalized group—to underlying health conditions or comorbidities or biased stereotypes, I write to you today as an alive and thriving disabled woman, one who lives in and contributes to her community, and as someone who questions the motives of those who attribute grave injustice toexploited or oppressed people’s own supposed deficiencies. Without a supportive partner to care for me in our home, I could as easily have died from neglect or COVID-19 in the average nursing home. My point here is to show that the long-term care industry is peddling this narrative simply to avoid responsibility for wrongdoing; that is, they want to pretend that people are dying in their facilities not because of the industry’s negligence, greed, or malfeasance, but instead because disabled and older people have a particular tendency to die en masse. The narrative in ‘Care for Our Senior’s Act’ is yet another example of the industry’s connivery and manipulation (I will append a brief example at the end of my testimony to show how they advance this narrative by playing with statistics).
Generally speaking, when any group of people are marked as suspect or inferior in some manner, when they are segregated and denied the resources and liberties that others enjoy, their flourishing will indeed be impeded, and they will be at a greater risk of contracting infections or disease. This is evidenced throughout history from the decaying and dank tenement houses of the early 19th century, the horrific conditions of the Warsaw ghetto, to the abuses that occurred in state institutions for people with disabilities. Given a deadly pandemic combined with deplorable (or at best unsafe) conditions, where people are segregated and treated as fungible objects from which to extract government benefits (or cheap labor), even AHCA and LeadingAge lobbyists like Mr. Mark Parkinson or Mr. David Gifford might be at a mortality risk 630 times higher than 18 to 29 year olds not forced to endure similar circumstances. (The industry’s claims are rarely supported by evidence, and with brief examination, can be shown inaccurate. Their act is at best slipshod and indicates an arrogance reinforced by years of overindulgence and a lack of accountability.)
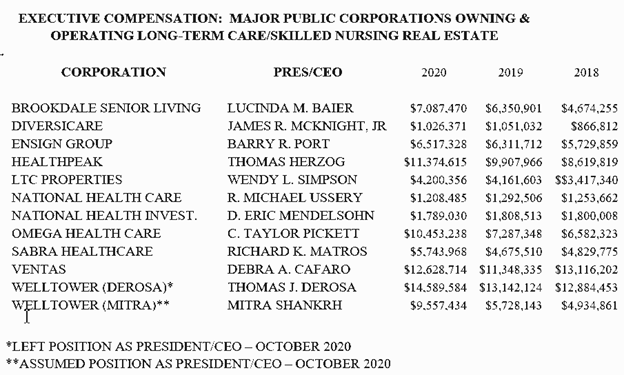
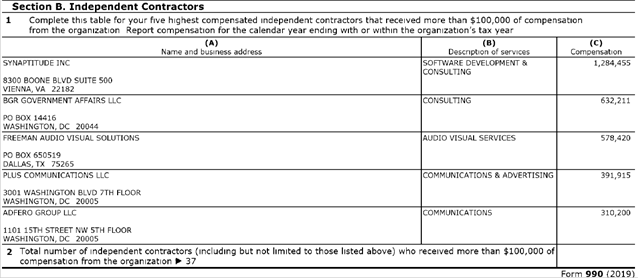
In contrast to those who are key players on K Street or spend most of their time in boardrooms or lobbying in the halls of Congress, I want to emphasize that my perspective is informed by my advocacy work in nursing homes where I have spent a great deal of time. I form bonds with residents. I know many of their spouses and children’s names, where they were from, the hobbies they enjoyed, and the kind of work they did. All of this they generously shared with me. I learned what it was like working in a Pennsylvania textile mill in the 1930s, surviving a chemical plant explosion in Texas and the revolution in Cuba, and growing up in Mexico in the 1940s. I have heard stories from war brides from France and Vietnam or the time a woman had to sew thousands of sequins by hand on her daughter’s quinceanera dress. I feel myself privileged to be granted the opportunity to listen. And unlike CEOs who earn $1,427,192 for lobbying, state ombudsman programs rely on volunteers. I have dedicated my life to this issue and yet rare is the occasion that I am asked to contribute to this topic. I—and other disability justice activists—have not been lavished the same platforms to speak given to long-term care industry CEOs and lobbyists. As a result of this, the voices of significantly disabled people, those at imminent risk of institutionalization or those in institutions, are squelched by the industry narrative. When I initially started out as ombudsman, I applied the principle of charity to the industry’s narrative, but with careful appraisal of the incongruity between what residents, families, ombudsmen, advocates, experts, HHS regulators, CNAs, CMS, and the OIG evidenced compared to the industry’s slant, it became apparent that industry representatives either have a deficient understanding of the culture and operations their business practices engender, or worse, they are impervious to the suffering of disabled people. Choosing not to see injustice or corruption, however, seems contrary to their lofty mission statements and commitments they have made to taxpayers.
On occasion, circumstances force us to confront the ugliness and brutality that inevitably festers where we sequester vulnerable people; stories of abject cruelty rip away the veil of inattention we cultivate to block from our view the relentless mill of everyday abuse, neglect, and hopelessness. In these moments of outrage, we perceive the true nature of institutionalization and perhaps even what we must do, but those flashes of insights quickly fade. Soon those with vested interests haul out the timeworn reform narratives and “bad apple” scapegoats that persuade us to look away again, to participate in systemic neglect from afar.
As a LTC ombudsman I could not simply look away from the toll of daily abuse and neglect residents experience or ignore their justified feelings of abandonment and the despair it begets. My ombudsman work bears out what ought to have long been obvious to any attentive person, namely, that segregating people in institutions can never foster or indeed ever permit equal treatment.[1] Nor—as over a hundred years of disability history attests[2]—can this model be fixed through reform. We cannot fix that which, by its nature, leads to systemic human rights violations. Severing people (like older and disabled people) from their homes and communities necessarily devalues them as persons and citizens. The diminishment is felt immediately. The freedoms they enjoyed vanish as institutional regiments constrict the courses of their lives. These utilitarian routines deprive them of their privacy and autonomy for the sake of efficiency and cost-effectiveness. Confined in these facilities without the projects and relationships that endowed their lives with meaning and shaped their social identities, they experience a kind of social death.[3] And so too their former communities, continuing on without them, lose the connection to them as full persons still deserving of the moral consideration and respect we are obliged to confer on those people in the community. Isolated, powerless, and dehumanized, people institutionalized inevitably suffer grave harms, not only from abuse and neglect, but from the very act of banishing them from the moral communities that granted the rights and benefits they are now denied.
To be sure, congregate institutions try to simulate community to hide these realities, but such ersatz contrivances are no substitute for genuine social inclusion and belongingness; the simulations are parodies. Such a model cannot produce “person-centered care” no matter how many CMS regulations we enact and enforce. Nor can quarterly congressional hearings and regulatory tweaks—informed by the usual actors they serve to benefit—amount to anything more than theater, political performances that strike those people who must endure the injustice as thoughtless cruelty.
Only a transformative shift in public policy can end these injustices. This shift will require scrutinizing narratives widely considered axiomatic. These include the beliefs that institutionalization is an unavoidable consequence of aging and disability, that institutions provide safer environments (a claim long used to rationalize the barbarity of social removal despite evidence demonstrating the contrary), that uprooting people from the homes, communities, and personal identities they spent lifetimes nurturing is compatible with our most revered social ideals, and finally that we can outsource our humanity—that is, our moral and social obligations to one another, including our disabled parents and children—as a revenue source for corporations and the workers they exploit and expect humane results.
By now, we know these outcomes of the institutional model; it is a model that objectifies deeply human concerns and favors economic values and imperatives such as competitiveness, efficiency, and profit margins, values that tend to attract predatory actors. And yet we persist with it, and one must ask why. Why do we continue to allow neglect, abuse, and dehumanization to go unchecked? Why do we allow those same predatory actors to manufacture and control the narratives that frame these issues, and indeed provide them platforms in the halls of Congress and in the media to influence unwitting advocates? Why do we persist with this cultivated naivety in the face of so much everyday suffering? The poor human rights records of congregate care facilities long predate the COVID-19 crisis, but the crisis has laid bare the preexisting conditions that led to deaths of over 181,000 disabled people in these institutions.
The horrors I witnessed as an LTC ombudsman keep me up at night, but also inform my disability justice work. And both my insomnia and activism partly derive from frustration. In deference to the industry, the system defangs oversight. I have fought countless nursing home attempts to involuntarily discharge residents only to have found that those residents, some with severe dementia, had disappeared the following week—to where, the nursing home curiously had (or at least offered) no clue. Sitting at their bedsides, I have held residents’ hands as they recounted instances of rape and abuse, often by staff. Residents have had limbs amputated due to a lack of wound care, understaffing, and poor training. I have seen residents gasp for air as nursing home staff rationed oxygen to save money. I have called Health and Human Services on multiple occasions for residents due to cruel instances of retaliation, only to leave the residents open for more of the same because they sought assistance from a deliberately debilitated regulatory system. Finally, I, myself, have been threatened on multiple occasions by staff and operators. Despite my notifying HHS regulatory and the Ombudsman Program, nothing of substance was done. To the industry, ombudsmen are gnats to swat away; they well know consequences will not be forthcoming. After all, there are few if any consequences for the negligent deaths of residents.
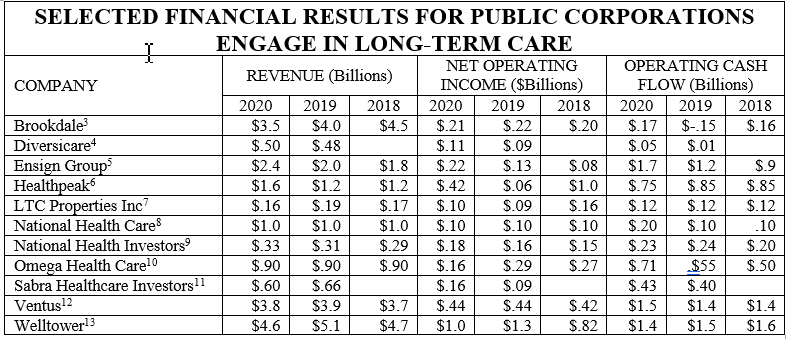
Culture change is impossible within the institutional habitus, particularly so when professional and agency advancement, corporate profit, race, age, and ableism are added to the brew. From the institutional point of view, the dehumanizing model is working as intended. Hence, pumping in ever more money to fund the same solutions and reforms will not bring about different results. As we have seen during the COVID-19 pandemic, nursing homes made record profits from taxpayer funded COVID subsidies, yet COVID cases and deaths, along with non COVID deaths resulting from inadequate infection control practices and severe understaffing, continued to rise.
There will be no substantive change until we end the Medicaid institutional bias by diverting taxpayer funds away from institutions and to programs that maintain or reestablish community integration. As I often explain, nursing homes are the most subsidized industry in the United States and increased monetary rewards serve only to entrench industry malfeasance. Diverting Medicaid dollars to fund HCBS not only reaffirms our commitments to the Americans with Disabilities Act (ADA), the Supreme Court’s Olmstead decision, and our professed democratic principles, it will also do more to soften the resolve of a recalcitrant industry (and similar nonprofits) than years of congressional hearings. In the long run, we will waste fewer resources on researching deficient industry practices and developing complex strategies to instigate change (only to be undone by lobbyists), on Office of Inspector General (OIG) and the U.S. General Accounting Office (GAO) investigations, on Ombudsman programs, on regulatory agencies to maintain the illusion of oversight, on healthcare costs resulting from the industry’s negligence, and on subsidizing the industry’s cost of doing business.
Sincerely,
Lydia Nunez Landry
Certified Volunteer Long-Term Care Ombudsman
Organizer for Gulf Coast Adapt
Appendix:
As promised, I want to briefly review a few of the rhetorical and statistical practices employed by the industry and their lobbyists to reframe the human catastrophe exacerbated by the negligent practices in LTC facilities. The author of Care for Our Seniors Act, which aspires to learn from “tragedy” and implement bold solutions, concedes that LTC facilities were the epicenter of the “once-in-a-century” pandemic’s ravage. The force-of-nature language distances the 170,000 deaths (now up to 181,286 deaths) from any culpable agent. And indeed, no one is to blame for the virus, just as we can blame no one for a major flood. But we can blame them for negligent and habitual substandard practices (such as not maintaining levees) that substantially worsen the toll. The author mentions “independent research” by “leading…experts” which shows that “COVID-19 outbreaks in nursing homes are principally driven by the amount of spread in the surrounding community.” The only actual research offered—conducted in May, 2020, long before the vast majority of cases occurred—did conclude that size and location of facilities were factors while traditional metrics such as star ratings and prior citation for poor infection control were not. (Most of the citations were articles from industry magazines, one of which mentioned the article just cited.) It’s unclear how this exonerates the industry. Moreover, the study, thus interpreted, becomes an outlier, as much more research has found direct links between poor quality ratings and significantly higher numbers of COIVD cases and deaths (see here and here).
Instead of dueling studies, we might focus on statistics. The author notes another force of nature behind the deaths, namely time: aging and the fragility of bodies. The virus just happens to target the frail and elderly adults with underlying health concerns that live in their facilities. The author incorrectly asserted that the average age of nursing home residents is 85, but correctly asserted that most residents have underlying conditions, as indeed most people over 65 years old have multiple chronic conditions, in and out of LTC facilities. First some numbers:
The U.S. has approximately 52 million citizens aged 65 or greater. Of them, 430,000 have died from complications of COVID-19 infections. Of those, 130,000 died in nursing homes—the author mentioned 170,000 deaths, but that includes congregate facilities the data from which is sparse, so I shall stick with the 130,000 in nursing homes (NHs). Thus, 300,000 died elsewhere than a NH. NHs warehouse approximately 1.4 million residents, ~ 90% of whom are 65+ years old. The total number of cases in NHs is, at the moment, 643,314, and, for non-NH people in the same age group, 2,666,625. Looking at the bare infection and death numbers, one might think that nursing homes did well—too well, in fact, for the author’s contentions.
But consider again that most people over 65 years old have chronic conditions and most people, even with their bleach wipes, have rudimentary infection controls in their homes. Now, 9.28% of the 1.4 million people in NHs have died from COVID; we can round that up to 1 in every 10. But if non-NH people in the same fragile age group died at that rate, we would have an incredible 4,342,857 more deaths than we do, as only 1 in 167 non-NH elderly people died from COVID. Indeed, examining only those infected, you are nearly twice as likely to die (20% vs. 11%) if you’re in a NH than not. Indeed, the infection rate in NHs is 46% vs. 5.3% for non-NHs fragile people.
Now, ultimately, industry spokespeople will claim that the deaths occurred because all these people are interacting in close quarters, and so on. But this is not something that can be fixed, and so it underscores why we need to turn back to community integration instead of warehousing people in admitted death traps.
[1] See, for example, Liat Ben-Moshe, Decarcerating Disability: Deinstitutionalization and Prison Abolition (Minneapolis, MN: University of Minnesota Press, 2020).
[2] Sara F. Rose, No Right to Be Idle: the Invention of Disability, 1840s–1930s (Chapel Hill, NC: The University of North Carolina Press, 2017).
[3] Jana Králová, “What Is Social Death?” Contemporary Social Science 10, no. 3 (2015): pp. 235–248, https://doi.org/10.1080/21582041.2015.1114407.