By:
Dave Kingsley
Everyone But the Totally Uninsured Receives Government Subsidized Medical Care. Only the Poor are Stigmatized
Practically all medical care in the U.S. is subsidized by federal and state governments – mostly by the federal government. The taxes to pay for these subsidies are collected from workers’ paychecks, sales taxes on what they buy, and property taxes that are paid by homeowners or added into rent/lease payments. And yet, it is only Medicaid, a medical care program for the poor, that is stigmatized. But the poor pay taxes too. Indeed, a disproportionate share of taxes.
The biggest tax subsidy is awarded to companies providing health insurance for their employees. When companies can write down their federal income taxes, they are actually getting money from the government – they are legally allowed to keep money that they owe the government. That is why these “breaks” are called tax expenditures.
Indeed, the $251 billion in tax write downs for corporations providing health insurance is the largest tax expenditure by far.[1] Furthermore, this deduction is a transfer of wealth from lower income Americans (who earn their employee benefits) to wealthier classes who increase their assets from equities and compensation in the healthcare industry. In costing labor, employers trade benefits for wages. In fact, in many negotiations in which I was on the negotiating team, we often settled wage disputes by offering to “sweeten the health insurance package.”
The poor pay more than their fair share of taxes that keep governments running. In the U.S. taxes on capital have been continuously reduced while at the same time taxes on consumption and labor have increased. This puts the heaviest burden on the lowest income groups and lightens higher income groups’ tax load. Nevertheless, Medicaid recipients are treated like freeloaders and “lesser thans” while everyone receiving other forms of subsidized healthcare are considered solid, upstanding Americans by politicians blaming poor people and the elderly for budget deficits.
“What We Do unto the Least of These”
Capitalist America as it has evolved can be harsh and unforgiving for the unfortunate, which could be any of us. With job loss, we can find ourselves struggling to keep a roof over our head and food on the table. At the very least we could lose our health insurance. The Affordable Care Act is not affordable for the unemployed. If you live in a state that has not expanded Medicaid, i.e., has not made residents with incomes below 120% of poverty eligible for Medicaid, you must have children and be in extreme poverty to qualify. If not, you will not be eligible for any healthcare program.
Let’s say a person lives in a state that has expanded Medicaid. And let’s say that person lives in a so-called “red state” like Arkansas or Missouri. The governors and legislators of those states will humiliate them and create administrative barriers to establishing eligibility for no other reason than they assume they are a cheater until they prove otherwise. These legislatures are dominated by pious Christians who despise poor people despite their prophet’s admonishment “what you do unto the least of these; you do unto me.” It is easy to bully poor people for the purpose of impressing constituents with bravado about controlling wasteful spending.
The poor are despised by right-wing politicians and a large portion of Christian America. Certainly, we don’t see the powerful Christian Church Industry – otherwise known as “faith based” institutions – closing ranks to take up the cause of their less fortunate brethren. Their prophet did that but for the most part they seem reticent about exerting their influence.
Transfer of Wealth from the Poor to the Wealthy
Conservatives claim that poverty in the U.S. is far lower than officially measured by the federal government due to transfer in the form of welfare such as Medicaid, child tax credits, and the Earned Income Tax Credit. There are several problems with the conservative wealth transfer argument. First, the poor struggle day-to-day to survive due to paltry benefits and continued threats of loss of those benefits and actual loss due to administrative complexities that are hard to navigate in a hostile political environment.
Second, transfers to the poorest of the poor are paltry compared to the transfers to the upper classes in the form of such mechanisms as capital gains write downs, untaxed cash flow, earnings on unrealized gains, and investments in tax free municipal bonds – to name a few “loopholes” for the rich. The hypocrisy of politicians claiming to save “we the people” money by bullying poor people on Medicaid is palpable in legislatures these days. Congresswoman Vicki Hartzler of Missouri is a wealthy owner of an Agri Corp that receives hundreds of thousands of dollars in undeserved federal farm subsidies. Nevertheless, she is a loud voice for clamping down on benefits for the voiceless, the powerless, and the defenseless who need those benefits for their health and often for their very survival.
WATCH FOR UPCOMING BLOG POSTS:
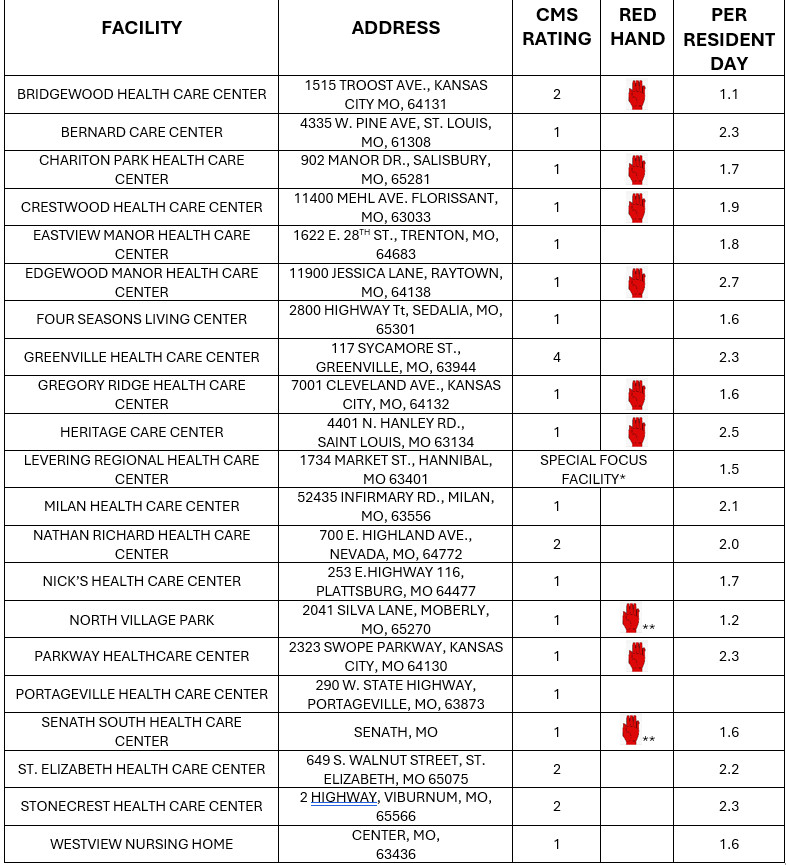
“Lucrative Medicaid Funded Nursing Home Care”
“Finding the Roots of Medicaid in the History of Slavery & Jim Crow”
“Corporate Medical Care Benefits: The Privatization of Medicaid”
“The Poor as a Government Healthcare Class: A Uniquely American Idea”
“The Injustice of the ‘120% of Poverty Gap’ in States That Have Not Expanded Medicaid”
[1] Tax Expenditures | U.S. Department of the Treasury. Other big tax expenditures include the mortgage interest deduction, and a variety of corporate real estate write downs, including depreciation. There is no doubt that the tax codes are a major factor in the maldistribution of wealth.